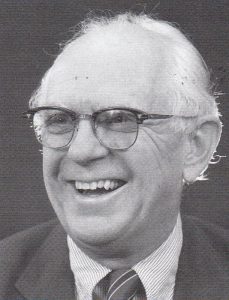
Belding H. Scribner, or “Scrib” to his many friends across the world, died after a fall from his houseboat in Seattle on June 19, 2003. With his passing, nephrology lost not only one of its true giants but a colleague of extraordinary gentleness, humility, and integrity who made unsurpassed contributions to our field.
In 1960, Dr. Scribner, working with Wayne Quinton and David Dillard, perfected the Scribner shunt, a Teflon device that allowed patients for the first time to be connected repeatedly to hemodialysis machines thereby launching the era of modern renal replacement therapy as well as the clinical discipline of nephrology as we now know it. For that accomplishment, Dr. Scribner shared with Willem Kolff the 2002 Albert Lasker Award for Clinical Medical Research, considered the American equivalent of the Nobel Prize, for “the development of renal dialysis, which changed kidney failure from a fatal to a treatable disease, prolonging the lives of millions of patients”[J Am Soc Nephrol 13:3027–3030, 2003].
Belding Scribner was born January 18, 1921 in Chicago and attended Williams College, the University of California at Berkeley, and Stanford University School of Medicine, where he received his M.D. in 1945. At Stanford he fell under the mentorship of Dr. Thomas Addis who first introduced him to the challenges of kidney disease. He completed a residency in internal medicine at the San Francisco General Hospital followed by a fellowship in medicine at the Mayo Clinic. While at the Mayo Clinic, Dr. Scribner first heard of the experience with the Kolff-Brigham rotating drum artificial kidney from a lecture by John Merrill.
Recruited to Seattle by the legendary Robert Williams, he joined the faculty at the University of Washington in 1951 and became the first Head of the Division of Nephrology at that institution in 1958, a position he held for 24 years. He became an Emeritus Professor of Medicine at the University of Washington in 1990 and held the Belding H. Scribner Endowed Chair in Medicine from 1984 until his retirement in 1991. After retirement, he returned to the Division of Nephrology weekly for several years to continue teaching his highly popular fluid and electrolyte balance classes to medical students.
Dr. Scribner’s contributions to nephrology went far beyond the work which first made chronic dialysis possible. In the ensuing years, he eagerly shared this new technology with physicians from around the world who came to Seattle to learn how to provide chronic dialysis to their patients. He spent the remainder of a productive career working tirelessly on multiple aspects of end-stage renal care, ranging from improving the technology of dialysis treatment to both general medical and societal issues that were created by this new and growing population of patients with end-stage renal disease. He and his group at the University of Washington were at the forefront in both defining, and designing successful treatments for, the multiple medical problems that beset patients with chronic renal failure, including anemia, renal osteodystrophy, and accelerated cardiovascular disease. He pioneered home hemodialysis/self care. Intermittent peritoneal dialysis was perfected as a treatment modality with development of new machines for overnight peritoneal dialysis. The Tenckoff catheter was developed by Henry Tenckoff while working in Dr. Scribner’s program at the University of Washington. Dr. Scribner’s vision of the “artificial gut” led to the development of the Broviac-Hickman, later the Hickman, catheter in Seattle and formed the basis for much of what is now routine total parenteral nutrition therapy.
Dr. Scribner believed strongly that dialysis should be done primarily in a setting outside the hospital, should never be done for profit, and should be universally available. Neither the Scribner shunt, nor any of the technical developments in dialysis that followed it, were ever patented. In 1962, together with Dr James Havilland, then President of the King County Medical Society, Dr. Scribner developed the first non-profit, outpatient dialysis facility in the United States, the Seattle Artificial Kidney Center, which has since grown into the still-non-profit Northwest Kidney Centers with 12 satellite facilities that dialyze over 1000 patients in the Seattle/Puget Sound area. In 1962, he also helped to establish the first anonymous lay committee to make decisions regarding the allocation of scarce and very expensive dialysis resources to those who would profit most from them. This mechanism for dealing with a complex ethical issue has often been referred to as the beginning of the modern discipline of bioethics, and Dr. Scribner has been called the “father of bioethics.” Finally, with the support of Senators Henry Jackson and Warren Magnuson from Washington, Dr. Scribner was instrumental in persuading Congress in 1972 to pass legislation creating the Medicare End-Stage Renal Disease Program which ensured that all Americans who needed it would have access to chronic dialysis therapy.
Throughout his career and during his retirement, “Scrib” was an inveterate tinkerer who worked continuously not only on improving dialysis technology but also on flying his beloved radio-controlled model airplanes from the deck of the houseboat in Seattle that he shared with his wife Ethel. He was one of the outstanding leaders in nephrology during our time. In addition to the Lasker Award, other honors included serving as President of the American Society of Artificial Internal Organs (1964) and of the American Society of Nephrology (1978), membership in the Institute of Medicine, fellowship in both the American College of Physicians and the Royal College of Physicians, and the receipt of many awards, including the John Peters award from the American Society of Nephrology, the Jean Hamburger award from the International Society of Nephrology, the David Hume award from the National kidney Foundation, the Torchbearer award from the American Kidney Fund, an award from the Gairdner Foundation, and many others. He held honorary degrees from the University of Göteborg and the Postgraduate Medical School of London.
In addition to his beloved wife, Ethel, Dr. Scribner is survived by seven children, six grandchildren, and millions of patients around the world whose lives, or those of their loved ones, were saved or made better by his contributions.